The Development and Causes of Cancer (Cancer development)
Cancer development
Introduction
Simply put, cancer is the result of unregulated cell division. Cancer cells divide when they should not divide, should not stop when they stop dividing, and should not a populate when they are apoptotic. In the worst case, cancer cells leave the area where they appear and move to other parts of the body.
Cancer cells look or act like normal cells from which they originate. Then the question comes: Why do cancer cells behave so badly? The result is the genes of the affected cells. In cancer cells, changes in key genes cause cells to function abnormally. These changes are usually the result of changes in DNA(mutation) in the cell. Because there are many factors that can cause mutations, the same amount of factors can cause cancer to occur.
The development of cancer occurs in a multi-step process. As cells become more abnormal, they acquire new abilities, such as the ability to release growth factors and digestive enzymes. The cells continue to divide, affecting nearby normal cells and generally reducing the function of the affected organs. Even abnormal cancer cells sometimes a populate, so a large enough tumour may take several years to reach. While not all cancers share the exact same steps, many types of cancers share some general characteristics in their development. More information on this topic can be found in most basic biology books, and we recommend the eleventh edition of Campbell Biology.
The content of this chapter:
- The beginning, promotion and development of cancer
- Tumour development stage
- Cancer stem cell
- Looking for cancer stem cells
- Cancer stem cells and treatment
- Summary of chapters
The beginning, promotion and development of cancer
In the eighteenth century, London doctor Percival Pott was the first to discover the relationship between cancer and environmental factors. He noted that the incidence of scrotal cancer is high among people who sweep chimneys. He speculated that this was caused by exposure to coal and tar. He observed a two-stage model of cancer development in observation: 1) initiator and 2) promoter. Pott has observed in many years of observation that many chemicals, radiation sources, viruses and bacteria are involved in the development of cancer.
The initial experiment was performed on animals. Researchers have tested the ability of chemicals that react with DNA and non-reactive compounds to cause cancer. The model used was mouse skin cancer. In this system, researchers applied test chemicals to the skin and observed tumour growth. The researchers found that DNA-reactive substances cause tumour formation only when the experimental animal is exposed to another non-reactive substance. Compound is reacted with DNA and in some ways alter the genetic composition of a cell is referred to mutagens (mutagen). Mutagens that cause tumours to produce tumours are called initiators. Non-reactive compounds that stimulate tumour development are called promoters. About 70% of known mutagens are also carcinogens – compounds that cause cancer. “Complete carcinogen” (Complete carcinogen) both the initiator and accelerator are, as may occur in tumor development without the use of another compound.
Initiation
“Initiation” is the first step in a two-stage model of cancer development. An initiator that has not yet reacted with DNA is altered (usually electrophilic) by a drug metabolizing enzyme in the body, and then causes a change (mutation) in the DNA. Since many initiators need to become active through metabolism, initiators are often specific to a particular tissue type or species. The role of the initiator is irreversible; once a particular cell is affected by the initiator, it is more susceptible to promotion until it dies. “Starting” is the result of a permanent genetic alteration. Any daughter cells that are produced by the division of mutant cells will also carry mutations. In the study of mouse skin cancer development, a linear relationship between the dose of the initiator and the amount of tumour has been observed. Thus, exposure to an initiator increases the risk and the risk increases indefinitely with higher levels of exposure.
Promote (Promotion)
Once the cells are mutated by the initiator, they are susceptible to promoters. These compounds promote cell proliferation and produce mutant cells resulting from many initiators. If the organism has not been previously treated with an initiator, the accelerator has no effect.
Unlike initiators, promoters do not covalently bind to DNA or macromolecules within cells. Many receptors bind to the surface of the cell to influence the intracellular pathway leading to cell proliferation. There are two main types of promoters: specific promoters that interact with receptors in a target cell or target cell that determine tissue; and non-specific promoters that alter gene expression without the presence of known receptors. Promoters are usually specific to a particular tissue or species. Because they interact with receptors that exist in different amounts in different tissue types. Although the use of accelerators and the risk of tumour growth are dose dependent, the promoters have a measurement threshold and maximum effect. Very low doses of the promoter do not cause tumour development, and very high doses do not create more risk than moderate exposure.
Development (Progression)
In mice, repeated promoters can cause benign papilloma on the skin exposed to the initiator. Most papillomas degenerate after treatment has stopped, but some have further developed into cancer. The frequency of progression indicates that additional, spontaneous mutations are obtained in papilloma that develops into cancer. The term progress is coined by Leslie Foulds, a process in which benign tumours are gradually transformed into new and malignant tumours. Progress is associated with karyotypic changes because almost all “progressive” tumours are aneuploid (with the wrong number of chromosomes). This karyotype change is associated with increased growth rate, invasiveness, and metastasis, and is associated with biochemical properties and morphological changes. 5
Stage of cancer development
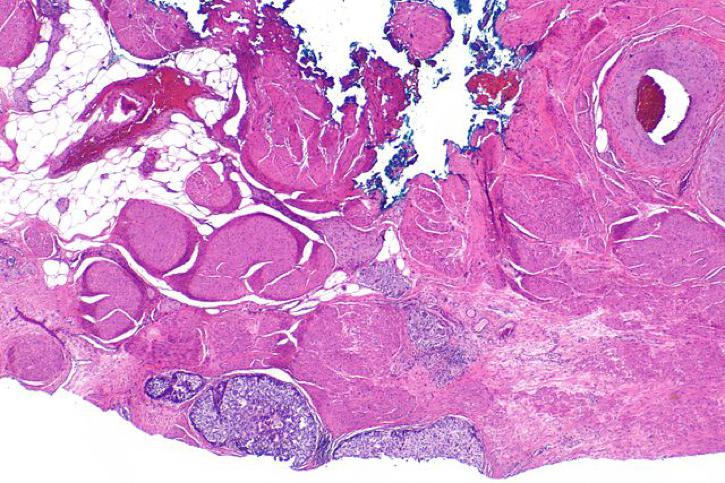
The development of a single gene-mutated cell into a tumour is a gradual process. The procedure described below is applicable to solid tumours such as epithelial cancer or sarcoma. The development of blood cell tumours also undergoes a similar process, but since blood cells can float freely, they are not restricted to fixed locations in the body.
Proliferation – Mutated cells divide in an uncontrolled manner, resulting in an excess of cells in the tissue region. The cells still have a normal appearance, but the amount is too much!
Structural abnormalities – More genetic changes in proliferating cells result in more and more abnormal growth. Cells and tissues don’t look normal any more. Cells and tissues may become disordered.
In situ tumours – more changes make cells and tissues more abnormal. The cells now spread over a larger area, and the tissue regions involved are mainly composed of mutated cells. These cells tend to “degenerate” or gain more primitive abilities. For example, a liver cell no longer produces a liver-specific protein. This type of cell is dedifferentiated or “retired.” The key to in situ growth is that the cells stay in the initial position and have not passed through the basal layer to invade other tissues. This type of cancer can usually be completely cured by surgery because the abnormal cells are all in the same location.
This type of tumour has not yet invaded adjacent tissues. Based on similar cases and microscopy, such growth is generally considered to have the potential to gain invasiveness and is treated as malignant growth.
Cancer (malignant tumours) – These tumours have the ability to invade surrounding tissues and/or spread (metastasize) to areas outside the tissue. These metastatic tumours are the most dangerous and account for many cancer deaths. The next few sections will detail some changes and capabilities that make cancer cells form large tumour tissue and transfer to other parts of the body.
Some tumours do not develop to the extent that they invade distant tissues. This tumour is considered benign . They are not considered to be cancerous because they do not spread beyond their original location. Benign tumours are not as fatal as malignant tumours, but they can still cause serious health problems. Large benign tumours may put pressure on organs and cause other problems. In the case of brain tumours, the space inside the skull is limited, which means that large tumour growth in the brain cavity can be fatal.
More information on this topic can be found in Chapters 13, 14 of The Biology of Cancer by Robert A. Weinberg.
Cancer stem cell
What is a stem cell?
Stem cells are a special type of cell that can accurately copy itself (also known as self-renewal )and can change (differentiate) into many specialized cell types in the body. Specialized cells produced by stem cells include nerves, muscles, and cells on the inner wall of the digestive system.
Stem cells are not very active in most parts of the body. In some locations, including the gastrointestinal tract, stem cells continue to divide and differentiate to replace shed or dead cells. Stem cells also play a role in healing damaged tissues.
Below is a video of how stem cells can complete their self-renewal and differentiation processes. This process is called “asymmetric cell division” and it ensures that stem cells are always available when needed.
The existence of cancer stem cells (CSCs) was predicted decades ago, but recent studies have identified cancer stem cells in a variety of cancer types, contributing to extensive research in this area.
Where did the cancer stem cells come from?
In theory, cancer stem cell CSCs can be formed in a variety of ways. Mutations can occur in differentiated cells (ie, skin cells), causing cells to reverse or “degenerate” into cells with some stem cell capabilities. Cancer stem cells can also be formed by normal stem cell cancer. Researchers have used skin cells to create cancer stem cells in the laboratory . The researchers used the virus to activate specific pathways and to characterize the stem cells of the target cells. Studies have shown that normal cells can become stem cells after a specific series of mutations.
The probability that any particular cell develops a series of mutations that cause cancer is relatively low. Cell types that are affected by most cancers, such as epithelial cells, have a very short life span and are even less likely to accumulate all the required mutations. Normal stem cells are long-lived, they are more likely to accumulate to the necessary mutations and may be a source of cancer stem cells.
What is the difference between the cancer stem cell hypothesis about the origin of cancer and the traditional view?
The cancer stem cell hypothesis suggests that only a small fraction of cells can be transformed into cancerous cells. In other words, only a very small number of cell populations in tumortumours lt in continuous, uncontrolled growth observed in cancer.
The traditional view of the origin of cancer predicts that any cell can acquire mutations that result in uncontrolled replication. Likewise, all cells in the tumour are predicted to be able to divide indefinitely.
Search for cancer stem cells
What led to the study of cancer stem cells?
There are several reasons why researchers have determined that the cancer stem cell hypothesis is convincing. The frequent failure of cancer stem cells for cancer treatment, the large number of cells required to cause cancer growth in model organisms, and other theoretical differences in cancer development provide a reasonable explanation. The identification and isolation of cancer stem cells is a big challenge. Researchers have discovered some cell surface proteins (also known as markers) on cancer cells with important stem cell functions. These markers include CD44, CD133 and ALDH1. 7
One of the evidences supporting the existence of cancer stem cells is that when the researchers observed the tumours they appeared to contain several differentiated cell types. Traditional theories about cancer development can explain this, but the large number of mutations required to create such a mixture is unlikely to occur. For example, if a tumour is formed by a single mutant cell, the tumour will contain only that type of cell, not many types of cells:
If multiple cells of different types in the same region are mutated, this will result in a tumour of mixed cell type:
Cancer stem cells have the ability to produce many types of cells, resulting in a mixture of cells found in tumours:
Statistically, the probability of a stem cell turning into a cancer stem cell is much higher than the probability of multiple gene mutations in multiple cells in the same region leading to cancer with multiple cell types.
Cancer stem cells and treatment
What is the impact of cancer stem cells on treatment?
Current treatments “target” cancer by acting on actively dividing cells. Most drugs work by inducing death of cancer cells (through apoptosis). Cancer stem cells carry mutations that cause cancer, but they do not necessarily divide rapidly. This relatively inactive state will enable them to evade the effects of cancer treatment, which explains the frequent recurrence of cancer. Cancer stem cells (CSCs) also effectively repair DNA damage and avoid apoptosis, making them difficult to treat with current drugs. We can compare this escape from treatment to weeds in the garden. Cancer stem cells are like the roots of weeds, and most tumour masses are the leaves and stems of weeds. Removing the visible part of the weed seems to kill it, but the roots of the ground quickly grow new stems and leaves, and the weeds continue to grow.
Why is it difficult to target cancer stem cells?
The problems that clinicians encounter when treating cancer are the same as those encountered when treating cancer stem cells with anticancer drugs. Because normal stem cells and cancer stem cells are very similar, it is difficult to kill cancer stem cells without harming normal stem cells. Drug resistance is another major obstacle to the treatment of cancer and cancer stem cells. Stem cells often have high levels of specific cell pumps (ie, multi-drug resistant proteins, MDR) that are capable of expelling cancer drugs from cells, rendering the drug less effective. Stem cells are also more difficult to kill than normal cells because they have the ability to block the signal that drugs, such as chemotherapy, cause cell death (apoptosis). Excessive anti-apoptotic proteins help stem cells to evade the effects of cancer treatment.
Learn more about multidrug resistance proteins (MDRs) and drug resistance.
Learn more about cancer cell death (apoptosis).
Summary of cancer development
Introduction
- All of our cells have similar structures and most functions.
- Cancer can be divided into five basic types based on cell type:
- Epithelial cell tumour – epithelial cells
- Sarcoma – muscle, bone, cartilage, fat or connective tissue
- Leukaemia – blood cells or their precursor cells
- Lymphoma – cells from the bone marrow; cancer affects the lymphatic system
- Myeloma – specific blood cells; B lymphocytes (B cells)
Stage of tumor progression
- Progression of the tumor is usually carried out step by step:
- Hyperplasia – excessive cell division, but normal appearance
- Structural abnormalities – abnormalities in tumor cells and tissues
- In situ tumor – the tumor mainly contains mutated cells and is growing up; it does not leave the place of origin
- Malignant tumor – the tumor has begun to invade nearby or distant tissue
- Benign tumors stay in their original position and do not invade other tissues.
Initiator and accelerator
- “Initiation” is the first step in a two-stage model of cancer development.
- Initiators cause irreversible changes (mutations) in DNA that increase the risk of cancer.
- Promoters are the second step in a two-stage model of cancer development.
- Once a cell is mutated by an initiator, it is susceptible to an accelerator.
- Promoters increase cell division in two main forms:
- Specific – through receptors acting on or in target cells
- Non-specific – alter gene expression without known receptors
Carcinogen
- The substance that causes cancer is called a carcinogen.
- The process of cancer development is called cancer.
- Long-term exposure to specific carcinogenic chemicals is associated with an increased risk of a particular cancer.
- One of the most effective carcinogens for humans is benzopyrene, a compound of cigarette smoke.
Virus and bacteria
- Certain viruses and bacteria are also associated with the initiation and promotion of tumor growth.
- Some viruses directly cause cancer by affecting cell division, while other viruses cause cancer by causing chronic inflammation or reducing immune system function.
Chronic inflammation
- Chronic inflammation is an important factor in tumor development.
- Inflammation can lead to altered cellular behaviour, promoting blood vessel growth (angiogenesis) and tissue reorganization.
- Markers of inflammation are associated with worse treatment expectations for cancer patients.